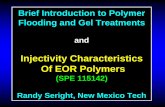
Polymer Poster Symposium MCB Retreat Spring 2014 · 2014-02-18 · Polymer Poster SymposiumMCB...
Transcript of Polymer Poster Symposium MCB Retreat Spring 2014 · 2014-02-18 · Polymer Poster SymposiumMCB...

2
α-pPKC-θ (T538) Delivery via Cell Penetrating Peptide Mimics as a Novel Treatment of Aplastic Anemia E. Ilker Ozay1, Gabriela Gonzalez-Perez2, Joe Torres2, Gregory N. Tew1,2,3, and Lisa M. Minter1,2,3
1Molecular and Cellular Biology Graduate Program, 2Department of Veterinary and Animal Sciences, 3Department of Polymer Science and Engineering, UMass Amherst, Amherst, MA, 01003
Polymer Poster Symposium MCB Retreat Spring 2014
Aplastic Anemia (AA)
Factory for all blood cells
Bone marrow In aplastic anemia (bone marrow failure),
§ Bleeding § Infection
Autoimmune disorder “Aberrant T helper-1 (Th1)
lymphocytes” Immune-mediated
destruction Th1 Th1 Th1
Current Treatments
§ Bone marrow transplantation
§ Anti-thymocyte globulin administration
§ Blood transfusion
Molecular Signaling in Aberrant Th1 Cells
IFN-γ
T-BET
IL-2
NOTCH1IC PKC-θ
§ Protein kinase C-θ(PKC-θ) gets phosphorylated in
activated Th1 cells (Threonine 538 residue for full activation)
Roderick et al., JEM 210, 1311-1329, 2013; Young, N.S. & Maciejewski, J., N Engl J Med 336, 1365-1372, 1997 1
Rationale behind targeting PKC-θ • Intact PKC-θ signaling is necessary to facilitate disease progression in the mouse model of aplastic anemia. • The disease can be completely rescued using Rottlerin by inhibiting PKC-θ function in the mouse model of aplastic anemia. • The viral immunity can still be protected in PKC-θ knockout mice. • Current treatment for aplastic anemia includes Anti-thymocyte globulin administration for Th1 cells targeting surface markers. However, 30-40% of the cohorts do not respond to this therapy.
Inhibits the phosphorylation
of PKC-θ, thereby its activation
Matsumoto et al., Immunity 23, 2005; Springael et al., Biochem Pharma, 2007; Solomou et al. Blood, 2006; Scheinberg et al., The Journal of Pediatrics 153, 2008.
2
Targeting PKC-θ: Using An*bodies to Inhibit Its Func*on
PKC-θ IS A POTENTIAL THERAPEUTIC TARGET FOR BONE MARROW FAILURE
TREATMENT.
INHIBITING PKC-θ FUNCTION IS BENEFICIAL TO TURN DOWN
ABERRANT TH1 CELL ACTIVITY IN APLASTIC ANEMIA.
STRATEGY
PKC-θ T538
α-pPKC-θ PKC-θ
T538
α-pP
KC
-θ
Interfering with the function
Cell Penetrating Peptides (CPPs) § Peptides which have the ability to internalize a cargo into cells.
HIV-1 TAT
RKKRRQRRR!49- -57
§ Guanidinium-rich domain § Covalently attached to cargo § Responsible for cellular uptake
§ More efficient than other cationic CPPs
§ Preferable to lysine
Polyarginine
PEP-1
§ Better uptake § Both hydrophobic and lysine-rich § Also non-covalent interactions
Sgolastra,F., deRonde, B.M, Sarapas, J.M., Som, A., Tew, G.N.; Accounts Chem. Res. 2013. ASAP; Stanzl et al., Accounts Chem. Res., 2013, ASAP; Kurzawa et al., Biochimica et Biophysica Acta 1798, 2010, 2274-2285; Morris et al., Nature Biotech. 19, 2001, 1173-1176
3
T-cell Master Key
CPPM
Inspired by; HIV-1 TAT, Pep-1, and Polyarginine
Design of Cell Penetrating Peptide Mimics (CPPMs)
CPPMs are able to enter and deliver a bioactive
cargo to T cells
Research Aim and Questions
Forming a complex of CPPMs and α-pPKC-θ (T538) and delivering them into T cells (hPBMCs) to neutralize PKC-θ activity both in
vitro and in vivo with the eventual goal of treating AA
§ Can we deliver α-pPKC-θ (T538) by using our CPPM?
§ Can cell-penetrating α-pPKC-θ (T538) neutralize the actions of PKC-θ in vitro?
§ Can in vivo delivery of α-pPKC-θ (T538) attenuate immune-mediated bone marrow failure in a “humanized” mouse model?
4
Delivery of CPPM/α-pPKC-θ into T Cells
Blank Agent1/FITC-IgG CPPM/FITC-IgG
Comparison between commercial agent and CPPM
5
Population shifted to higher fluorescence with CPPM
α-‐pPKC-‐θ
WITHOUT CPPM
α-‐pPKC-‐θ
WITH CPPM
Acknowledgments & Funding Lisa M. Minter Gregory N. Tew Barbara A. Osborne Tew Lab
Federica Sgolastra Brittany M. deRonde Bob Fu Michael Lis Katie Gibney Cathy Walker Joel Sarapas Madhura Pawar Coralie Backlund
Minter Lab Gabriela Gonzalez-Perez Christina Arieta Kuksin Joe Torres Karthik Chandiran Wesley Rossiter Victoria Mello Jessica Jarmolowicz Osborne Lab Rebecca Lawlor Anushka Dongre Furkan Ayaz Joseph Homsi Manit Munshi
Charles H. Hood Foundation for Child Health Research
12
§ We are able to successfully deliver α-pPKC-θ (T538) via our CPPM into hPBMCs
§ Our novel CPPM design has much better uptake of the antibody with compared to commercially available antibody delivery reagent
§ We are able to interfere with the actions of PKC-θ by observing reduction of T cell immune response marker expressions
§ AA model of mice treated with CPPM/α-pPKC-θ complex had longer survival compared to control mice
§ In vitro and in vivo studies of α-pPKC-θ (T538) delivery into hPBMCs have promising results for the treatment of aplastic anemia for clinical studies
Conclusions
11
In Vivo Humanized Mouse Model of Aplastic Anemia
10 9
6 7 8
In Vivo Humanized Mouse Model of Aplastic Anemia
NSG (NODscidIL2Rγcnull)
female mice
CPPM treated human PBMCs
Rest mice for 4 hours
Human PBMCs
CPPM/ α-pPKC-θ
Wait for 17 days γIR
CPPM treated mice lived LONGER (up to 36 days)
Gabriela Gonzalez-Perez & Joe Torres
41%
Mouse CD45
Human CD4
5
86% 92%
56% 88% 94%
Bone Marrow Spleen Peripheral Blood DMSO treated hPBMCs:
Bone Marrow Spleen Peripheral Blood CPPM/α-‐pPKC-‐θ treated hPBMCs:
11%
Human CD4
Human CD8
9% 20%
18% 15% 25%
Bone Marrow Spleen Peripheral Blood DMSO treated hPBMCs:
Bone Marrow Spleen Peripheral Blood CPPM/α-‐pPKC-‐θ treated hPBMCs:
54% 27% 70%
53% 28% 63%
Engraftment of Human CD45 Cells in Peripheral Tissues
Infiltration of Human CD4 and CD8 T Cells in Peripheral Tissues
0 10 20 30 400
20
40
60
80
100BlankRottlerinP13D5/α-pPKC-θ
Days
Surv
ival
(%)
DMSO Rottlerin CPPM/α-pPKC-θ
CPPM treated Humanized Mouse Model of AA
SURVIVAL STUDY
Gabriela Gonzalez-Perez & Joe Torres
T-cell Activation and Disease Markers In Vitro Experimental Design Cytokine Expression
CELLULAR VIABILITY AFTER 24 H OF TREATMENT
CD25-MFI
24h
48h
72h
0
2000
4000
6000
8000
10000
12000
**
*
*
Hours after Treatment
CD
25 (M
FI)
ns nsns
NOTCH1IC-MFI
24h
48h
72h
0
1000
2000
3000
4000
*
**
Hours after Treatment
NO
TCH
1IC (M
FI)
ns nsns
CD69-MFI (24 h)
Unstimulated
DMSO
Rottlerin
CPPM/α-pPKC-θ Treatment
0
200
400
600
800
1000*
CD
69 (M
FI)
**
T-BET-MFI
24h
48h
72h
0
500
1000
1500
2000
***
**
Hours after Treatment
T-B
ET (M
FI)
ns ns ns
IFN-γ
24h
48h
72h
0
10000
20000
30000
40000
*
ns
***
Hours after Treatment
IFN
-γ c
once
ntra
tion
(pg/
mL)
nsns ns
IL-2
24h
48h
72h
0
1000
2000
3000
4000
5000
**
ns *
Hours after Treatment
IL-2
Con
cent
ratio
n (p
g/m
l)
n/a ns ns
0
20
40
60
80
100ns
*
Cel
lula
r via
bilit
y (%
)
CD25%
24h
48h
72h
0
20
40
60
80
100
*
***
nsns ns
UnstimulatedDMSORottlerinCPPM/α-pPKC-θ Treatment
Hours after Treatment
CD
25+ %
Cel
ls
CD25%
24h
48h
72h
0
20
40
60
80
100
*
***
nsns ns
UnstimulatedDMSORottlerinCPPM/α-pPKC-θ Treatment
Hours after Treatment
CD
25+ %
Cel
ls