SEPSIS
description
Transcript of SEPSIS

SEPSISIntern Bootcamp
Scott Denstaedt, PGYIII

Sepsis /ˈsɛpsɨs/; from the Greek σῆψις: the state of putrefaction and decay

Background
• local inflammation systemic inflammatory response tissue hypoperfusion and multi-organ failure DEATH– release of specific toxins eg. Gram Negative Bacteria
lipid A, Staph. aureus TSST-1– Host cytokine response eg. TNF-alpha
• Septic shock with multi-organ failure is most common cause of death in ICU
• >750000 cases/year, mortality rate of 1 in 4

***Sepsis is a spectrum of illness that requires early intervention to prevent complications and progression***

Definitions• Systemic Inflammatory Response Syndrome
(SIRS) criteria– response to infectious and non-infectious insults– 2 criteria needed to meet SIRS– Temp >38, <36– HR >90– RR >20, PaCO2 <32 (differs depending on textbook)– WBC >12k or <4k or 10% bands
• *NO BLOOD PRESSURE IN SIRS CRITERIA

Definitions
• Sepsis– 2 SIRS criteria + source of infection (you don’t
necessarily need concrete evidence – high level of clinical suspicion is enough)

Definitions• Severe Sepsis
– Sepsis with organ dysfunction (don’t memorize the list below)• Sepsis-induced hypotension• Lactate above upper limits laboratory normal• Urine output <0.5 mL kg/h for more than 2 h despite adequate fluid
resuscitation• Acute lung injury with PaO2/FiO2<250 in the absence of pneumonia as
infection source• Acute lung injury with PaO2/FiO2<200 in the presence of pneumonia as
infection source• Creatinine[2.0 mg/dL (176.8 lmol/L)• Bilirubin[2 mg/dL (34.2 lmol/L)• Platelet count <100,000 lL• Coagulopathy (INR >1.5)

Definitions
• Septic Shock– Sepsis induced hypotension despite adequate
fluid resuscitation• Sepsis induced hypotension = SBP <90mmhg or
40mmhg change from baseline

• Each term describes the the intensity of infectious insult• Increase in # of SIRS criteria associated with decreased interval
to progression of severe sepsis and septic shock

***CAVEATS***
• Elderly, uremic, and patients with end-stage liver disease or those receiving corticosteroids may NOT have fevers.
• SIRS Criteria are entirely non-specific– EG. Everyone met SIRS criteria on day one of
intern year• Clinical picture must be taken into account


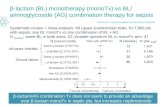
Rivers et. al 2001
• Initial 6 hours of resuscitation in ED
• ~1-1.5 hours to identification of sepsis on avg.

Early Goal Directed Therapy Outcomes
• Severe Sepsis and Septic Shock– Randomized to standard therapy (iv fluids, abx) v.
Early Goal Directed Therapy• RESULTS (Patients with EGDT):– Elevated CVP, MAP, Scv02– Decreased Lactate– Improved Mortality (almost 50% reduction in
mortality compared to standard therapy!!)


Surviving Sepsis Campaign
• Global initiative to reduce mortality from sepsis
• Evidence based guidelines for the management of sepsis
• Evidence graded based on LEVEL OF RECOMMENDATION (strong v. weak) and QUALITY OF EVIDENCE (ABCD)
• First published 2003, revised 2008, revised again 2012

• Diagnosis:– 2 sets of blood cultures from separate sites (culture ALL
vascular devices unless <48 hours old) BEFORE antibiotics (1C)– Imaging studies promptly performed to confirm potential
source (UG)• Antimicrobial Therapy:
– Administration of effective antimicrobials within 1 hour of recognition of septic shock (1B) or severe sepsis (1C)
– Initial empiric therapy against all likely pathogens and that penetrate adequately into tissue presumed to be the source of sepsis (1B)
– DAILY reassessment for de-escalation (1B)• Source Control:
– seek and diagnose a source - if possible remove it within 12 hours (1C)

• Initial resuscitation:– Protocolized resuscitation (Early Goal Directed
therapy) during first 6 hours (1C)– Abnormal lactate should be re-checked, and
normalization sought (2B)– Crystalloids initial fluid of choice (1B)– Hydroxyethyl starches for fluid resuscitation
should not be used (1B)– Albumin in severe sepsis and septic shock in
patients who require substantial amounts of crystalloid (2C)
– Initial fluid challenge = 30ml/kg (1C)– Continue fluid challenge technique as along as
there is hemodynamic improvement (UG)

• Vasopressors:– Norepinephrine initial pressor (1B) – Epinephrine added to or as substitute for
norepinephrine (2B)– Vasopressin 0.03 added to NE to reach MAP or
decrease dosage of NE (UG)– Dopamine only in highly selected patients (due to
risk of arrhythmia) (2C)– Pheynlephrine only if arrhythmia with NE or as a
salvage therapy (1C)– Low dose dopamine for renal protection should
not be used (1A)– All patients on vasopressors should receive
arterial catheters (UG)

• Steroids:– NO STEROIDS if initial resuscitation
(fluid/pressors) adequate. If this is not achievable, we suggest intravenous hydrocortisone alone at a dose of 200 mg per day (2C).
• Blood product administration:– transfuse only when Hgb <7g/dl to target of 7-9 in
the absence of extenuating cricumstances (1B)– FFP should not be used to correct coagulopathy in
the absence of bleeding or planned procedure (2D)
– transfuse prophylactically when platelets <10k or <20k if significant risk of bleeding, goal of >50k if active bleeding, surgery or invasive procedure (2D)

• Mechanical ventilation (ARDS)– another lecture all together
• Sedation:– minimize sedation and titrate to sepcific endpoints 1B– Neuromuscular blocking agents avoided if possible if no ARDS
1C• Glucose control:
– initialize protocolized glucose management when 2 blood glucose levels >180 (insulin gtt), target goal <180 1A
• DVT prophy and Stress ulcer prophy:– LMWH when possible in severe sepsis 1B, Dalteparin if CrCl <30– PPI or H2RA in severe sepsis, septic shock 1B
• Nutrition:– enteral or oral feeding as tolerated in first 48 hours 2C
• Goals of care:– set goals of care 1B– address as early as feasibile, no later than 72 hours after
admission 2C

2008 compared to 2012
• Crystalloid initial fluid of choice• Epinephrine 2nd pressor of choice• Dopamine no longer recommended• Activated protein C no longer recommended• Normalization of lactate as an endpoint in sepsis
induced hypoperfusion• Use of 1,3-B-D Glucan and antigalactomannan
antibodies if concern for invasive candidal infection

Your Septic Patient: H+P
• age• infectious review of systems: fever/chills, fatigue,
myalgias, cognition, HA, sensitivity to light, rhinorrhea, sore throat, neck stiffness, cough, sob, cp, n/v/d, abdominal pain, back pain, dysuria, frequency, skin changes or wounds, recent sick contacts, recent antibiotics
• medical comorbidities (chronic diseases etc.)• medications: immunosuppressants

Your Septic Patient: Exam
• vitals Temp, HR, RR, BP (stable or not)• head and neck (meningeal signs, oropharynx,
sinuses), cardiac (murmurs!), respiratory (signs of consolidation), back (CVA, spinal/paraspinal) tenderness, abdomen, ascites, skin exam for wounds, feet!

Your Septic Patient: Labs• WBC - %PMN, %bands• Hgb and Plt (important for sepsis and DIC)• BUN/Cr• Anion Gap• LFT (Hyperbilirubinemia in sepsis, also shock liver)• INR (to assess for DIC)• Lactate if hypotension, anion gap, ill appearing• ABG if anion gap, hypoxic, obtunded (pH <7.2-7.25 -->
patient belongs in ICU)• U/A, Urine culture• Blood cultures from two different sites• Culture other sites as necessitated by history and exam

Your Septic Patient: Imaging
• CXR• Other imaging depending on your clinical
suspicion (usually CT with contrast)

Your Septic Patient: Treatment
• Empiric therapy based on suspected source of infection
• Supportive Care– Early Goal Directed Therapy– Surviving Sepsis Campaign, update 2012

Clinical Method
• Identify your septic patient (based on the definitions)
• Triage level of care (Floor v ICU)• Work-up and treat their underlying infection• Resuscitate according to EGDT and Surviving
Sepsis Campaign– Initial fluid resuscitation 30mL/kg as fast as
possible, unless CHF/low EF• If in MICU place central line, arterial line


Clinical Pearls• Managing Sepsis on the floor:
– Use defined endpoints for fluid resuscitation• U/O >0.5cc/kg/hr• MAP >65• Normalization of lactate
• KNOW the patients Ejection Fraction and renal function• Fluid resuscitation is the priority!!!• Start pressors if MAP <65, even if CVP not yet known• Transfer to MICU:
– Hypotension resistant to fluid resuscitation (Septic shock) – usually after 4-6L fluid
– Severe lactic acidosis (pH 7.2-7.25) – Severe or acutely worsening hypoxia or obtundation

Sources
• Rivers et. al Early Goal Directed Therapy, NEJM 2001
• Dellinger et. al Surviving Sepsis Campaign 2012, Intensive Care Med 2013
• Current Diagnosis and Treatment: Critical Care, 3rd Edition
• http://www.youtube.com/watch?v=MceGURfXdR0